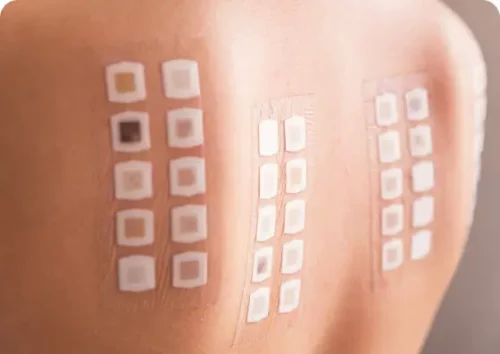
Allergy Patch Testing
Allergy patch testing is a common test used to confirm the cause of allergic contact dermatitis.
learn more
 go back
go back
Angioedema is swelling under the skin that can affect various parts of the body and treatment varies patient-by-patient. Angioedema often resolves without therapy.
Make An AppointmentAngioedema is swelling that occurs just beneath the skin in the body. It can happen in many areas of the body and not just the external regions that we usually associate with ‘skin.’ For example, angioedema can also occur in the uvula, the throat, and the larynx, as well as in the intestines or the genitals.
Skin
Angioedema also often occurs on the face, arms, legs, feet and hands. This condition commonly happens in tandem with hives, a rash that can appear spontaneously on the skin and that is triggered by a histamine response in the body. The swelling in angioedema feels as if large, firm, and thick welts have formed under the skin. This swelling can also cause redness, pain at the site, or even a small amount of heat in the affected areas.
Intestines
When angioedema occurs in the intestine, it can cause stomach pain. When it occurs in the throat or other areas associated with respiration, angioedema can affect a patient’s breathing, making it difficult to get enough oxygen.
Treatment
In these scenarios, a patient with angioedema needs to seek out medical help immediately. In milder cases, angioedema can resolve on its own.
There are four different types of angioedema, each associated with different causes.
Allergic angioedema is the most common form of the condition, often triggered by foods such as shellfish, fish, peanuts, tree nuts, eggs, and milk.
In some cases, allergic angioedema is caused by environmental triggers. These triggers can include but are not limited to pollen, animal dander, insect stings, and latex. Identifying the trigger of allergic angioedema is an essential part of treating the condition.
While associated with an allergic reaction, allergic angioedema may have a genetic component as well. This type of the condition occurs most often in areas of the body that have loose areas of skin, including the face, throat, limbs, and genitals.
Hereditary angioedema, or HAE, is a very rare type of the condition. HAE occurs when the patient’s body is unable to produce enough C1 esterase inhibitor. The deficit in this blood protein causes the body to allow more fluid to move out of the blood into adjacent tissues. This, in turn, results in the swelling associated with angioedema.
Most patients with HAE experience their first episode of angioedema before the age of 12. As a genetic condition, patients with HAE are at a high risk of passing it onto their own biological children.
A condition similar to HAE can occur in those over 40 with weakened immune systems. This type of angioedema, known as acquired angioedema, has the same symptoms as HAE, but is not genetic and cannot be passed down to biological children.
The second type of angioedema is drug-induced angioedema. In this subtype of the condition, a patient’s angioedema is triggered by medications. Medications that can cause drug-induced angioedema include penicillin, aspirin, and NSAIDs, including naproxen and ibuprofen.
ACE inhibitors used to treat high blood pressure can also trigger an episode of angioedema. While patients may have a lifelong reaction to medicines such as penicillin, angioedema triggered by ACE inhibitors can occur suddenly even after taking the medicines safely for extended periods of time.
It is estimated, however, that such reactions to ACE inhibitors only happen in less than one percent of patients and may be associated with the buildup of a vasodilator in the blood.
In some cases, doctors may not be able to identify the cause of angioedema. In these situations, the condition is referred to as idiopathic angioedema. While the exact cause of idiopathic angioedema cannot be confirmed, it may be associated with the following triggers:
This type of angioedema can occur anywhere on the body, but it is most likely to appear around the lips and the eyes. Only in very rare cases can it occur in the throat or mouth and cause respiratory difficulties. Some types of idiopathic angioedema will respond to treatment with antihistamines, even though the exact triggers are not known.
The most common symptom of angioedema is swelling and puffiness in the tissue beneath the skin. This can be accompanied by redness or blanching that turns white when pressed and then returns to a red color.
Patients with angioedema that presents with hives will also experience a red, bumpy rash at the sight of the swelling. Less common symptoms include patchy welts, dizziness, and pain or upset in the stomach.

What causes angioedema varies from type to type. Within each type, too, there are any number of triggers. Allergic angioedema is typically caused by allergens such as foods, pollen, insect bites, or latex.
Hereditary angioedema is caused by a genetic deficiency of a C1 inhibitor in the blood. Drug-induced angioedema can be triggered by any one of several medications, including ACE inhibitors and NSAIDs such as ibuprofen. Finally, those with idiopathic angioedema will not have a confirmed cause, but their condition may be triggered by causes as diverse as stress, exercise, or infection.
In most types of angioedema, the body creates a histamine response to a trigger, which then results in the release of excess fluid from the blood into adjacent tissues. This then triggers the swelling associated with the condition. The exception to this is hereditary angioedema, which is caused by the lack of C1 inhibitor in the body.
Diagnosing Angioedema typically involves taking a medical history of the patient, including a history of any exposure to allergens or triggers. A doctor may also examine the skin for hives. Where allergic triggers are suspected, a patient may need to undergo additional testing to confirm a diagnosis in the form of:
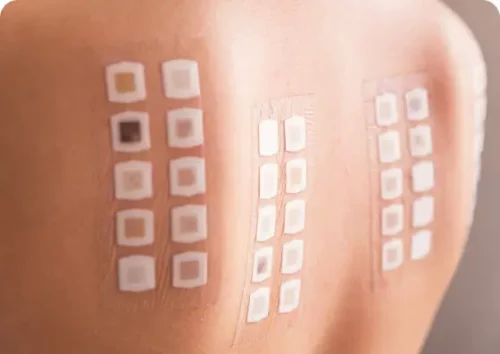
Allergy Patch Testing
Allergy patch testing is a common test used to confirm the cause of allergic contact dermatitis.
learn more learn more
Skin Allergy Testing
This is less invasive than blood tests and is a good alternative for patients who don’t like needles.
learn more learn more
Blood Testing for Allergies
Blood tests can tell if someone has allergies by finding antibodies in the blood that react to allergens.
learn more learn moreTreatment of angioedema varies from patient to patient and case to case. In many situations, angioedema will resolve on its own and patients will not require treatment. When cases of angioedema appear regularly or cause mild discomfort in a patient’s life, a doctor may prescribe an antihistamine if the patient’s angioedema is associated with a histamine response in the body.
Severe cases or chronic cases of angioedema may require stronger, prescribed medications, including corticosteroids like prednisone or immunosuppressants such as cyclosporine. These medications work to suppress the body’s immune response so that triggered inflammations are not as severe.
When patients go into anaphylaxis or respiratory difficulty as a result of angioedema, immediate medical attention is required. These patients may also need to carry and self-administer injected epinephrine in case they are exposed to a trigger. Anyone experiencing swelling in the throat or airways as a result of angioedema needs to consult with a medical professional right away.
Patients with hereditary angioedema are typically treated with esterase inhibitors, plasma kallikrein inhibitors, or bradykinin antagonists. These medications work to address the C1 deficiency in the body that causes hereditary angioedema. Most of these medications are delivered by subcutaneous injection and are approved by the FDA for self-administration by the patient.
Angioedema can resolve relatively quickly or last for longer periods of time. The duration of the swelling associated with angioedema depends on the patient and the type of angioedema involved. Generally speaking, most cases of this condition last anywhere from 1 to 3 days.
The best way to prevent Angioedema in cases that do not involve a hereditary cause is to prevent all exposure to a trigger. For example, if a patient’s allergic Angioedema is caused by pet dander, ensuring that the patient is never exposed to pet dander is the best way to prevent an episode. Those with idiopathic Angioedema may wish to make lifestyle changes that limit exposure to environmental triggers and reduce stress in general.
